There is limited information available at a national level about the burden of infertility in the United States. The
National Survey of Family Growth - 2011-2013 reports that 12.3% of all women age 15-44 report impaired fecundity - that is, they are not surgically sterile, yet find it difficult or impossible to get pregnant or carry a pregnancy to term. Among married, childless women of reproductive age, the proportion reporting impaired fecundity is almost a quarter (24.2%). In the NSFG, infertility - the inability to conceive - is only reported for married women. The NSFG reports that 6.1% of all reproductive-age married women are infertile, a proportion that increases to 13.5% among childless married women of reproductive age.
The CDC Divison of Reproductive Health, in consultation
with other governmental and non-governmental organizations, has released the
National Public Health Action Plan for the Dete
ction, Prevention, and Management of Infertility. The plan details the need to better understand the population-level issues that contribute to and cause infertility and may affect the health of a pregnancy. Specifically, it focuses on promoting healthy behaviors that can maintain fertility, encouraging prevention, early detection, and swift treatment of conditions that can threaten fertility, and reducing exposure to infectious, iatrogenic, environmental, and occupational exposures that can harm fertility. CDC has also released a grand rounds video titled
Time for Public Health Action on Infertility.
Sexually transmitted infections (STIs) such as chlamydia and gonorrhea, can cause pelvic inflammatory disease (PID), which in turn can lead to

infertility. As reported by the
National Chlamydia C
oalition, chlamydia is common in adolescents and young adults in the US, with an estimated 2.8 million new cases per year. One out of every 15 sexually active adolescent girls in the US has chlamydia. Twenty percent of untreated chlamydia infections result in PID, making this STI the leading cause of tubal factor infertility in the US.
CDC's 2015 STD Treatment Guidelines indicate yearly

screening of all sexually active females <25 years and older women at increased risk for infection for chlamydia and gonorrhea - a screening that the
National Commission on Prevention Priorities ranks as a high value, but underused clinical preventive service. Routine chlamydia screening could reduce the incidence of PID by up to 60%.
See the
2015 STD Treatment Guidelines site for a provider-focused pocket card and wall chart, as well as an app that combines information from the STD Treatment Guidelines as well as MMWR updates. For more information about chlamydia, including provider guidelines and resources, see the
National Chlamydia C
oalition. Of particular
interest may be their
Sexual Health Resource Exchange, where you can search and download customizable public awareness and education materials and share your resources.
Despite the fact that infertility is classified as a disease, only 15 states currently require any insurance coverage of infertility diagnosis or treatment, and only 8 of those mandate coverage of assisted reproductive technology (ART), such as in-vitro fertilization (IVF).
 Resolve: The National Infertility Association
Resolve: The National Infertility Association, which seeks to increase public awareness of infertility, provides patient and provider information, facilitates support groups, and advocates for access to all family-building options, released their 3rd annual
State Fertility Scorecard in August.
The Fertil
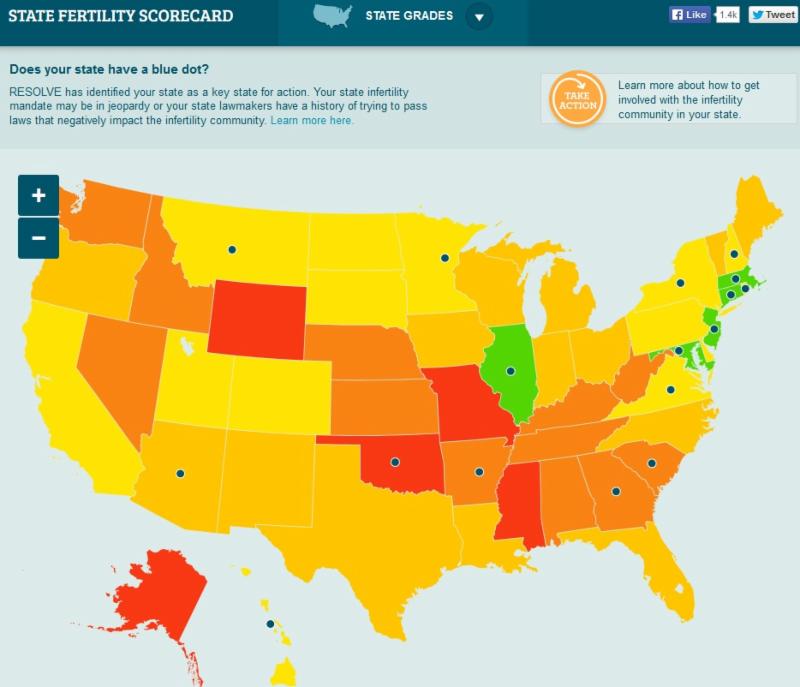
ity Scorecard evaluates states based on the number of peer-led RESOLVE infertility support groups; the number of fertility doctors at accredited clinics; the number of women in the state who experienced impaired fecundity; and state insurance mandates (or lack thereof). Additionally, blue dots were placed on states with pending legislation that could affect access to infertility diagnosis and treatment.
Assisted reproductive technology (ART), including treatments such as in-vitro fertilization (IVF), can provide people with infertility the chance to conceive, but also presents significant public health challenges due to the substantial risk for multiple birth delivery, which is associated with poor maternal and infant health outcomes. Even when elective single embryo transfer is appropriate, many couples choose to transfer multiple embryos per cycle. This is influenced by access to and affordability of treatment, as well as the desire to minimize the number of ART cycles experienced by the woman. Since most ART are not covered by insurance, couples have to pay the relatively high cost of the procedures out of pocket. For example, the median cost of a single IVF cycle in the US, including medications, is $19,200. As a result, many people are not able to afford treatment, while others are choosing to transfer multiple embryos per IVF cycle to increase the chances of success.
The
Fertility Clinic Success Rate and Certification Act mandate
s that all ART cycles performed in US fertility clinics are reported to CDC, which collects data on patient demographics, procedures, and outcomes per cycle in the
National ART Surveillance System (NASS). The latest surveillance summary from the NASS, published in MMWR -
Assisted Reproductive Technology, 2012 - details access to infertility treatment, pregnancy outcomes per cycle, and perinatal outcomes for the infants resulting from ART. Building on these national surveillance efforts, CDC, in

coordination with the Departments of Health in Connecticut, Florida, Massachusetts, and Michigan, has also established the
States Monitoring
Assisted Reproductive Technology (SMART) Collaborative. The goal of the SMART Collaborative is to strengthen the capacity of states to monitor ART-related maternal and perinatal outcomes using state-level data. The
Association of State and Territorial Health Officials (ASTHO) has a
fact sheet providing additional information about the SMART Collaborative and the initiatives in the four participating states.