 | |
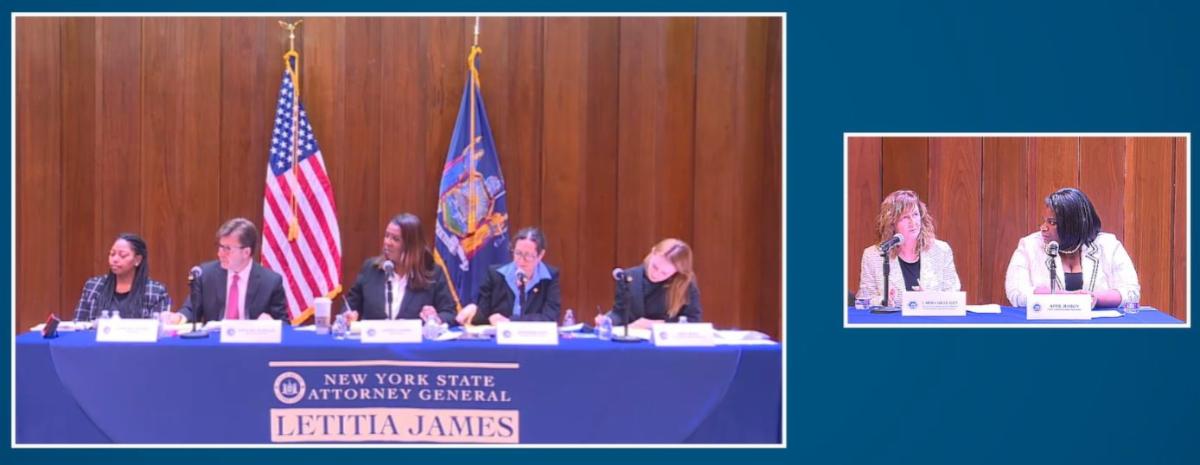
CLMHD Chair Presents Testimony at Attorney General Letitia James’ Public Hearing on Mental Health
On January 18, New York Attorney General Letitia James's office held its second in-person public hearing concerning the provision of mental health care for people with serious mental illness in the Western New York Region. The purpose of the hearing was to gain insight from the public regarding the problems people suffering mental health crises or chronic severe mental illness experience in accessing mental health services and use that information for legislative and enforcement solutions.
The Conference greatly appreciated the opportunity to have Chair, Laura Kelemen, LCSW-R, Niagara County Director of Community Services, present oral testimony at the hearing. Her testimony highlighted a variety of barriers to access to services, including workforce shortage, inadequate Medicaid reimbursement, and unavailability of hospital inpatient beds. Click here to read the written testimony.
Related: At hearing on mental health in Buffalo, NYS Attorney General says the system will be 'examined'
|  | |
Governor Hochul’s Bold Plan for Mental Health: Staffing Will Be a Key to Success
In her second State of the State address, Governor Kathy Hochul proposed significant investments in mental health with the goal of “fixing the entire continuum of care that is necessary to keep people safe and happy.” Her proposals range from expanding insurance coverage for mental health services to increased capacity for inpatient psychiatric beds. The plan also includes an expansion of outpatient services, payment parity for telehealth, more wrap around services for people transitioning from one setting to another, and expanded school-based mental health services. This holistic approach is commendable especially in light of the growing need for mental health services in recent years. A recent survey of psychologists reported increases in patients seeking treatment for anxiety, depression, and substance-related disorders compared with 2020. Caregivers reported an inability to meet the increased demand and that their patients were facing longer waitlists. Read more here.
|  | |
Governor Hochul Announces $38.2 Million Initiative to Address Street Homelessness
Governor Kathy Hochul on Tuesday announced the availability $38.2 million in state funding to establish eight Safe Options Support teams that will provide intensive outreach, engagement and care coordination services to individuals who are experiencing homelessness in areas of the state outside of New York City. Funded through the State Office of Mental Health, these teams will be modeled after ones now providing assistance to unsheltered individuals staying on the streets and within the subway system in New York City and will be deployed in areas of the state with high rates of street homelessness. Read more here.
| |
SAMHSA Releases Guide to Expanding Access to and Use of Behavioral Health Services for People At Risk for or Experiencing Homelessness
This guide highlights strategies for behavioral health and housing providers to conduct outreach and engage with individuals experiencing homelessness, initiate use of behavioral health treatment as they wait to receive stable housing and retain them in their recovery efforts once housed.
Related: SAMHSA Grants for the Benefit of Homeless Individuals
|  | |
Free Mental Health Crisis Care for Veterans Starts Tuesday across US
Starting January 17, any veteran who finds themselves facing a mental health crisis can go to the VA or any private facility for free. The government is hoping it can put a dent in the high suicide numbers that have plagued the military community for years (the US loses about 16 veterans daily to suicide).
Nick Stefanovic, the Director of Monroe County Veteran Services, said for a veteran in a mental health crisis, this is how it currently works: “You can go to a VA, and they will start the process of treating you and then quickly get you referred out to either private pay or something your insurance can cover,” he said. Read more here.
| |
NYAPRS/OMH Launch CORE Peer Navigator Hotline, Support Program Today!
The New York Association of Psychiatric Rehabilitation Services (NYAPRS) and the NYS Office of Mental Health (OMH) are excited to announce the launch of the CORE Peer Navigator Project. The CORE Peer Navigator Project is designed to engage and educate eligible individuals about New York State’s recent transition of four Adult Behavioral Health Home and Community Based Services (BH HCBS) to Community Oriented Recovery and Empowerment (CORE) Services. These services promote an individual’s recovery and personal empowerment in community settings. Read more here.
|  | |
SAMHSA Announces Funding Opportunities for Grants Addressing Substance Misuse, Substance Use Disorder Treatment on Multiple Fronts
The U.S. Department of Health and Human Services (HHS), through the Substance Abuse and Mental Health Services Administration (SAMHSA), is announcing Notices of Funding Opportunities (NOFOs) for five grant programs aimed at preventing substance misuse and treating substance use disorder (SUD) throughout the nation. The grant opportunities total about $73.4 million and align with the Biden-Harris Administration’s efforts to address the nation’s addiction and overdose crises. Read more here.
Related: New York State Department of Health Issues Latest County Opioid Quarterly Report Showing 14% Increase in Opioid Overdoses
|  | |
Out of Prison, But Struggling to Stay Healthy
Edward Johnson, 59, served 27 years in a Louisiana prison for bank robbery. “Prison is a brutal experience, and you have to find yourself and your path to maintain your sanity,” he says.
Released in 2016, Johnson has been trying hard to contribute to society, hoping to use the psychology degree he received in 2020. “I believe in transformation, a complete reversal, a process that gives you different values and principles,” he says.
But when he left prison, Johnson walked out bearing physical and mental health problems. Read more here.
|  | |
For Addiction Treatment, Longer is Better. But Insurance Companies Usually Cut It Short
Access to treatment for addiction has long plagued U.S. health systems. Why? Two reasons: It is expensive, and the long-term value of addiction treatment is often disregarded by insurance companies and other payers.
Its dirty little secret is that access to treatments that work are available to the few who can pay for it, while millions of Americans get substandard treatment or none at all.
From May 2021 to May 2022, more than 103,000 Americans died from drug overdoses. Yet treatment for substance use disorder (SUD) — and for mental illness as a whole — face limited covered benefits, delays in access to treatment, and denials of care at higher rates than medical and surgical care, despite federal efforts to drive parity for mental health, which extend back as far as 2008. Read more here.
|  | |
Working With ACOs To Address Social Determinants Of Health
Social, behavioral, and economic factors are important determinants of health and health outcomes. Many health care organizations are beginning to assess the social risks of their patients and facilitate interventions to address health-related social needs. Improving the integration of medical and social services is also central to the Biden administration’s health policy agenda. Organizations participating in payment models in which they are responsible for managing the total cost of care for assigned or enrolled populations, such as accountable care organizations (ACOs), may be particularly interested in integrating medical and social services. Read more here.
| |
A Look at Strategies to Address Behavioral Health Workforce Shortages: Findings from a Survey of State Medicaid Programs | |
The pandemic has exacerbated mental health and substance use issues and 90% of Americans believe the nation is in the midst of a mental health crisis. Despite increases in need, data show that treatment rates across all payers are low. Documented workforce challenges contribute to barriers in access to care and nearly half of the US population – 47% or 158 million people – living in a mental health workforce shortage
area. Behavioral health conditions (i.e. mental health and substance use disorders) are most prevalent in Medicaid enrollees, with data from 2020 showing that approximately 39% of Medicaid enrollees were living with a mental health or substance use disorder. Workforce challenges are widespread and go beyond Medicaid, but shortages may be exacerbated in Medicaid. Read more here.
| |
Round 3 of NYS Office of Strategic Workforce Development Grant Programs Now Open
On October 17, 2022, Governor Hochul announced the launch of New York State’s $150 million workforce development grant programs, administered by OSWD, that will support employer-driven, high-skilled workforce training programs. The first round of awards was announced in December 2022.
Round 3 of the OSWD grant programs is now open. Updated guidelines and materials can be found on the OSWD website. Applications will be accepted on an ongoing basis and awards will be announced every three months. The deadline for Q1 of 2023 is Friday, March 31, 2023, 11:59 PM.
| 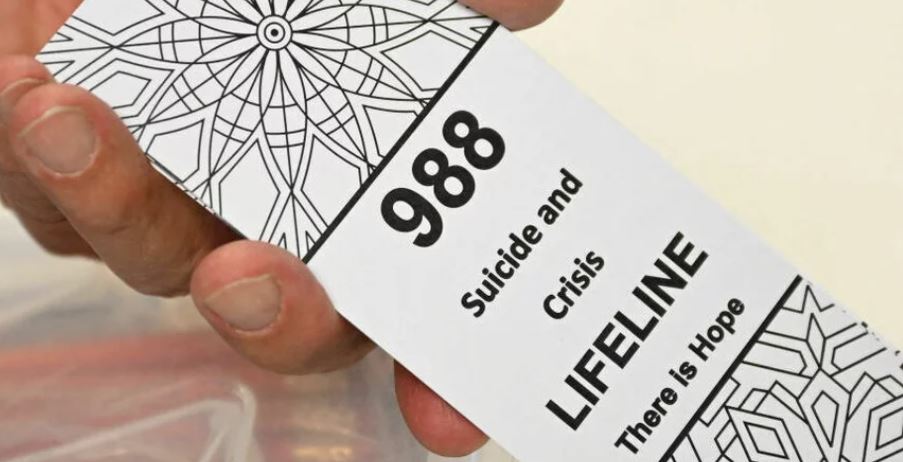 | |
988 Lifeline Sees Boost in Use and Funding in First Months
The 988 Suicide and Crisis Lifeline received over 1.7 million calls, texts and chats in its first five months. That's nearly half a million more than the old 10-digit Suicide Prevention Lifeline fielded during the same period the year before. Launched in mid-July last year, the 988 number is modeled on the 911 system and is designed to be a memorable and quick number that connects people who are suicidal or in any other mental health crisis to a trained mental health professional.
"We see the uptick in volume as an indicator that more people are aware of the service and are able to access it," says Kimberly Williams, the president and CEO of Vibrant Emotional Health, the non-profit that oversees the national 988 network of nearly 200 crisis centers spread across the nation. Read more here.
|  | |
UPCOMING EVENTS & TRAININGS
Supporting Providers of Color in the Pediatric Workforce: Practices to Diversify the Workforce and Improve Retention
January 19, 12 - 1:30 pm, Center for Health Care Strategies
Supporting Youth with High Acuity Crisis and Suicidal Needs
January 19, 2 - 3 pm, NASMHPD and Vibrant
988: It is NOT just a number- Webinar #1
January 20, 12:30 - 2:30 pm, National Academy of Sciences
988: It is NOT just a number- Webinar #2
January 23, 12:30 - 2:30 pm, National Academy of Sciences
Trauma-Informed Peer Support for Justice-Involved Peers
January 23 - 26, 1 - 4 pm, Mental Health Empowerment Project
PSYCKES for Health Homes and Care Management Agencies
January 24, 10 - 11:30 am, OMH
Housing as a Pathway to Justice: Engaging with the Local Community
January 24, 10 - 11:30 am, Corporation of Supportive Housing
Advancing Health Equity through Integrated Care ECHO - Q&A Session
January 24, 2 - 3 pm, National Council for Mental Wellbeing
Rapid-Fire Retention Strategies: How To Improve Behavioral Healthcare Provider Retention
January 25, 2 - 3 pm, Relias
Roundtable 2: The Experience of Mental Health Stigma Among Diverse Groups
January 26, 2 - 3 pm, OMH & Behavioral Health News
County Strategies to Recruit and Retain a Strong Behavioral Health Workforce
January 26, 2 - 3 pm, NACo
An aging undocumented population: Implications for complex care and communities
January 26, 3 - 4 pm, Camden Coalition
Where to Start: Getting Access to PSYCKES
January 31, 11 am - 12 pm, OMH
Reducing Jail Populations: Revisiting Technical Violations of Community Supervision to Decrease Jail
February 2, 2 - 3 pm, NACo
The Continuum of Care: Innovative Solutions for Addressing Complex Behavioral Health Needs
February 2, 2 - 3 pm, Behavioral Health Business
NYS OMH DFS Spotlight of Innovative Diversion Services
February 8, 10:30 am - 12 pm, OMH Division of Forensic Services
Diversity, Equity and Inclusion (DEI) Plus – Building a Culture of Inclusion
February 8, 1 - 2 pm, National Council for Mental Wellbeing
The Art of Talking to Teens about Substance Use
February 8, 8 - 9 pm, National Council for Mental Wellbeing
Data-Informed Care and Advocacy in Addiction Treatment
February 9, 2 - 3 pm, National Council for Mental Wellbeing
Navigating PSYCKES Recipient Search for Population Health
February 9, 2 - 3 pm, OMH
Using the PSYCKES Clinical Summary
February 15, 3 - 4:30 pm, OMH
| |
CLMHD CALENDAR
FEBRUARY
Executive Committee Meeting
February 1: 8 - 9 am
AOT Coordinators Call
February 7: 10 - 11:30 am
LGU Billing Staff Call
February 7: 11 am - 12 pm
Addiction Services & Recovery Committee Meeting
February 9: 11 am - 12 pm
Developmental Disabilities Committee Meeting
February 9: 1 - 2:30 pm
Mental Health Committee Meeting
February 9: 3 - 4 pm
LGU Clinic Operators Call
February 14: 10 - 11:30 am
CLMHD Membership Call
February 15: 9 - 10:30 am
Mental Hygiene Planning Committee Meeting
February 16: 1 - 3 pm
CLMHD Office Closed - Presidents Day
February 20
Children & Families Committee Meeting
February 21: 11:30 am - 1 pm
| |